Important Updates
- If you offer a drug plan to employees who are eligible for Medicare, you must take the following action by Oct. 15. Federal law requires you to tell your Medicare-eligible employees that their drug plan is creditable. Go to hmsa.com/creditable-drug-coverage1 for more information and to download the notice. If you have any questions, please contact your account representative or call 808-948-6377 or 1-866-726-9835.
- (IRS) posted to the Federal Register, "Extension of Certain Timeframes for Employee Benefit Plans, Participants, and Beneficiaries Affected by the COVID–19 Outbreak." 2 HMSA will adhere to the appropriate timeframe extensions related to COBRA, for those specific situations, until no longer applicable. The parameters of the COBRA law currently remain unchanged. For more information, visit the Help Center3.
June 2023:
Previously, the Biden Administration announced a definitive end to both the COVID-19 public health emergency (May 11, 2023) and the national health emergency (April 10, 2023). The U.S. Department of Labor, as allowed by the Joint Rule, subsequently exercised its discretion to determine July 10, 2023, as the end date of the Outbreak Period (60 days after the end of the public health emergency date, May 11, 2023).
- Individuals and plans with timeframes that are subject to the relief under the Notices will have the applicable periods under the Notices disregarded until the earlier of (a) one year from the date they were first eligible for relief, or (b) July 10, 2023 [the end of the Outbreak Period]. In no case will a disregarded period exceed one year.
- After July 10, 2023, the timeframes for individuals and plans with periods that were previously disregarded under the Notices will resume.
Glossary
A
Accreditation
The evaluation of a health plan
(for example, HMSA’s Health Plan Hawaii or Preferred Provider Plan),
health care facility, or program by a third-party organization to ensure
that specific standards are met. If the plan, facility,
or program meets those standards, it’s assigned an accreditation status.
Actual charge
The amount a provider bills the patient for medical services or supplies.
Administrative review
An approval process that an
HMO member’s
PCP or other health center
provider must request before services are rendered by in-state nonparticipating
providers and all out-of-state providers if no
HMSA participating providers
are available for the services needed. Without prior authorization
through this process, services provided by nonparticipating or out-of-state
providers won’t be eligible for benefits.
Advance directive
A legal document that tells your health care provider what kind of care you
want or don’t want if your medical condition prevents you from
making or communicating your decisions (for example, if you’re in a coma).
Alternative therapy
Healing techniques that use options other than conventional medicine.
For example, alternative therapies to quit smoking could include
hypnosis and laser therapy.
Anencephaly
A type of neural tube defect and serious birth defect where a baby is born without some of the brain and skull. This defect occurs when the upper part of the neural tube doesn’t close completely. Learn more about anencephaly.
Annual copayment maximum
The maximum deductible
and copayment amounts
you pay for most covered services
in one calendar year.
Annual deductible
The fixed dollar amount you pay each
calendar year before your
health plan will pay for certain services.
Appeal
Process available to providers and members to ask that a claim or precertification decision be reconsidered.
B
Baby blues
Having feelings of sadness, fear, anger, or anxiety occurring about three days after childbirth and usually ending within one to two weeks. Also known as postpartum blues, it's different from postpartum depression, a more severe, long-lasting form of depression. Behavioral health
The management or treatment of stress, depression, substance abuse, and
other behavior issues that affect an individual’s well-being.
Birth defects
Structural changes that a baby is born with that may affect any body part (heart, brain, arms, legs, face, etc.).
BlueCard® provider
A provider who participates with the
Blue Cross and Blue Shield Association
(BCBSA). HMSA is an independent licensee of the Blue Cross and Blue Shield Association.
C
Calendar year
The period starting Jan. 1 and ending Dec. 31 of any year.
Your first calendar year for a health plan begins on your effective date
and ends on Dec. 31 of that same year.
Centers for Disease Control and Prevention
Agency of the U.S. Department of Health and Human Services that
develops and conducts activities for disease prevention and control,
environmental health, occupational safety and health, and health education.
Certified nurse midwife
Is an advanced practice registered nurse who specializes in preventative women’s health maintenance and women’s reproductive health during pregnancy, childbirth, and postpartum.
Cesarean birth (c-section)
The delivery of a baby through a cut in the belly and uterus. Your ob-gyn may determine if you need a c-section to deliver your baby.
Chronic condition
An illness lasting three or more months,
as defined by the U.S. National Center for Health Statistics.
Chronic obstructive pulmonary disease
Permanent lung damage, often caused by smoking, in which airflow is
blocked and causes wheezing, coughing, and difficulty breathing.
COBRA
Consolidated Omnibus Budget Reconciliation Act of 1986.
A federal law that lets you and your eligible dependents pay for continued
health plan benefits if your plan ends because of a qualifying event such
as leaving a job or getting a divorce.
Coinsurance
The percentage you pay out of pocket for medical services and products
that are benefits of your health plan. Let’s say your plan has a
20% coinsurance for prescription drugs. If a prescription costs $100,
you’ll pay 20% and your health plan pays the remaining 80%.
Conception
This occurs when an egg becomes fertilized by the sperm. Conception needs to occur to become pregnant. Learn more about conception.
Information about you and the services that you received from a provider,
such as your symptoms, exam, test results, injury or illness, treatment,
and prescriptions. For more information about your privacy and rights,
our duties, and how CMI is used, see the
Notice to HMSA Members.
Coordination of benefits
Coordination of benefits: If you're enrolled in more than one health plan
(for example, you have health insurance through your job and your spouse's plan),
HMSA will apply rules to determine which plan pays first and which pays second.
Copayment
The dollar amount you pay out of pocket for medical services and products
that are benefits of your health plan. Let's say your health plan has a
$20 copayment for doctor visits. If a visit costs $100, you’ll pay $20
and your health plan pays the remaining $80.
Cost share
Also known as Other Brand Name Cost Share.
When you share in the cost of Other Brand Name drugs or devices,
the amount you pay is called the cost share.
You pay the cost share in addition to a copayment.
Coverage
The benefits that are provided according to the specific terms of your
health plan.
Covered services
Health care services and supplies that meet HMSA’s payment determination criteria and are described as covered in your Guide to Benefits.
D
Deductible
The amount you pay for medical services or products before your health plan pays.
Let's say you have a $1,000 deductible for hospital stays.
If a hospital bill is $5,000, you pay $1,000 to meet the deductible and your
health plan pays the plan benefit for covered services.
Dependent
People who can be enrolled in your health plan such as a spouse or child.
Disease management
A program for patients who have or are at risk for a specific
chronic condition.
Patients receive educational information and communication with health
professionals to help manage their condition. This preventive approach
decreases patients’ need for medical care and helps to improve
their quality of life.
Dual coverage
Coverage from two health insurance plans. For example, if you have two jobs,
you could be enrolled in health plans from both employers. If you're married,
you could be enrolled in your employer's plan and your spouse's employer's plan.
Durable medical equipment
Items that serve a medical purpose and can withstand repeated use,
such as wheelchairs, walkers and crutches.
E
Electronic health record (EHR)
Your medical records and health history filed in a computer or
stored online to help doctors provide you with proper care.
Eligible charge
The maximum amount that a doctor or hospital charges based on an agreement
between the provider and HMSA. Let's say your doctor charges $100 for office visits
(the actual charge), but HMSA negotiates a $75 eligible charge for doctor visits.
So the doctor bills you $75, you pay a portion of it (your copayment or coinsurance),
and we pay the rest.
Employee Retirement Income Security Act
The Employee Retirement Income Security Act, or ERISA, is a federal law
passed in 1974 that sets minimum standards for most voluntarily established
pension and health plans in private industry to provide protection for
individuals in these plans.
An employee benefit plan established or maintained by an employer or
by an employee organization (as that term is defined by ERISA), or
both, that provides medical care to employees and their dependents
directly or through insurance, reimbursement or otherwise.
End stage renal disease (ESRD)
Permanent kidney failure that requires dialysis or a kidney transplant.
F
Family plan
A health plan that you and your dependents, such as your spouse and children,
are all enrolled in.
Fetus
A developing baby in the uterus before it’s born (layman’s term). A developing offspring after the embryonic stage until birth. An unborn offspring.
Flexible spending account (FSA)
An account that your employer can set up so you can use pre-tax dollars
to pay for eligible expenses. Types of accounts include medical or dependent care.
You lose unspent money in the account at the end of the year.
A list of drugs that are covered under your drug plan.
G
Generic drug
A drug that works the same as a brand-name drug, according to the
Food and Drug Administration,
but costs less because it doesn’t have the same research and advertising costs.
Gestational diabetes
A form of diabetes that appears during pregnancy (gestation) in a woman
who previously didn’t have diabetes. Gestational diabetes is treatable,
especially if detected early in pregnancy.
Gynecologist
A medical doctor who specializes in caring for the reproductive system. A gynecologist doesn’t care for people who are pregnant and doesn’t deliver babies.
H
Called the Affordable Care Act (ACA), this law to reform the nation’s
health care system took effect in March 2010 to help more people get
affordable, quality health care.
Health center
A specified group of providers in the Health Plan Hawaii network that you
designate as your primary center of care. Your designated health center
is made up of your PCP and other providers.
Health Insurance Portability and Accountability Act
The Health Insurance Portability and Accountability Act of 1996 is a
law with several components. Title I addresses health care portability
to protect health insurance coverage for workers and their families when
they change or lose their jobs. Title II is designed to reduce the
administrative costs of providing and paying for health care through
standardization. It includes requirements to protect the privacy of
individuals’ health information.
Health maintenance organization (HMO)
A health care system used by plans such as HMSA’s
Health Plan Hawaii. HMO plans provide coverage for a wide variety of
health care services with an emphasis on
preventive care.
As an HMO member, you select a
PCP and health center
from the plan’s network.
All care you receive must be provided or arranged by your PCP except for
emergency care, HMSA’s Online Care, vision exams, gynecological exams,
and mental health and substance abuse treatment.
Health reimbursement arrangement (HRA)
An account that your employer can set up so you can pay for out-of-pocket medical costs.
Only your employer can put money into an HRA.
Health savings account (HSA)
An account that you or your employer can set up to save money tax-free
for medical expenses. The balance at the end of the year is
rolled over to the next year.
High blood pressure (also known as hypertension)
Having a blood pressure that’s higher than normal. A consistent blood pressure reading higher than 130/80 is considered the first stage of high blood pressure. A consistent reading higher than 140/90 is stage 2 high blood pressure. Seek medical attention immediately for a blood pressure reading of 180/120 or higher. Learn more about high blood pressure and how it can affect pregnancy.
High Density Lipoprotein
HDLs transport cholesterol from the body tissues to the liver, so the
cholesterol can be eliminated. HDL cholesterol is considered
the “good” cholesterol. The higher the HDL cholesterol level,
the lower the risk of coronary artery disease.
High-deductible health plan
A type of health plan with a high deductible (the amount you pay for services
before the plan pays). This plan typically has higher out-of-pocket costs and
lower premiums.
HMO home plan
Your HMSA group or individual HMO health care plan. Your HMSA plan is the
home plan when you are enrolled in the Guest Membership program.
HMSA works with the HMO host plan
to administer benefits while you’re away from home.
HMO host plan
A health care plan on the Mainland that provides you with a guest membership.
The host plan participates in the Blue Cross Blue Shield
Away From Home Care program and works with HMSA (your
HMO home plan)
to administer benefits while you’re away from home.
HMSA’s pharmacy benefit manager
HMSA’S pharmacy benefit manager provides a service contracted by HMSA to
process drug claims and administer HMSA’s mail-order drug benefits.
I
Immunization
The introduction of a vaccine or serum into a living organism to stimulate
the immune system, the body’s natural disease-fighting system, to
recognize invading bacteria and viruses and to produce substances
(antibodies) to destroy or disable them.
Individual plans
Health plans for people who don't have health insurance through a job.
You typically pay the entire amount of the monthly premiums.
Influenza
A virus infection of the upper respiratory system.
Most people who get the flu recover completely in one to two weeks.
However, some people develop serious and potentially life-threatening
medical complications. An annual influenza
immunization can help you
avoid getting the flu.
Inpatient
A patient who has been admitted to a hospital or other medical facility for
evaluation, treatment and observation, and requires an overnight stay.
L
Lifetime maximum
The maximum benefit amount set by HMSA that each member is eligible to
receive during their lifetime.
Low-birth weight
When a baby is born weighing less than 5 pounds, 8 ounces. Although these babies can be born healthy, some babies with low-birth weight can have serious health problems that need treatment.
M
Mail-order prescription
A prescription drug that you can order through the mail instead of at the pharmacy.
Mail-order programs deliver three-month supplies of drugs that are taken for
chronic conditions such as high blood pressure or high cholesterol.
Managed care
Organized system of health care delivery that manages cost efficiency,
health care quality, and provider accessibility.
Common managed care plans are the health maintenance organization
(HMO) and
the preferred provider organization
(PPO).
Maternity health care provider
A health care provider such as an advanced practice registered nurse (APRN) or physician’s assistant (PA) who works alongside an ob-gyn and provides specialized care in pregnancy and reproductive health.
Maximum allowable fee
The maximum amount that HMSA will pay for
covered services and supplies.
Medicare Advantage
Also known as Medicare Part C, this Medicare health plan is offered by
private insurers to provide hospital (Medicare Part A) and medical (Medicare Part B)
benefits. It typically offers more benefits than Original Medicare.
Miscarriage
The loss of the pregnancy before 20 weeks of gestation. Miscarriages are common and there are many reasons that miscarriages happen. Learn more about miscarriages.
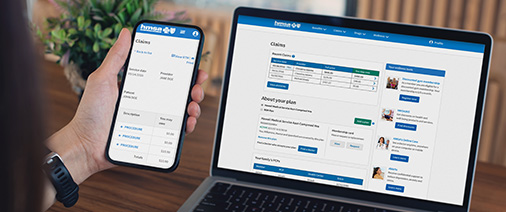
My Account
A secure area on HMSA’s website,
that helps you manage your membership with HMSA. My Account allows you to
access information about your own plan and claims, download HMSA forms,
and use helpful tools.
N
National Committee for Quality Assurance
An independent, not-for-profit organization that evaluates how well a
managed care organization
meets quality standards.
Its accreditation process is
nationally recognized for improving health care access and quality.
Network
Also called provider network. A group of physicians, hospitals, and other
health-care professionals who are under contract with HMSA. HMSA negotiates
payment rates with the network to provide services to its members.
Neural tube defect (NTD)
A type of birth defect that occurs very early in pregnancy. The neural tube makes up the early brain and spine in the fetus. The two most common NTD is spina bifida and anencephaly.
Nicotine replacement therapy
The use of nicotine patches, nicotine gum, and other nicotine products as
part of a smoking-cessation program.
Nonparticipating provider
A provider who is not under contract with HMSA.
A doctor, hospital, pharmacy, lab, or health center that doesn’t have a
contract with HMSA to charge set rates. Using these providers almost
always costs more than using participating providers.
O
Ob-gyn
A medical doctor who’s both an obstetrician and gynecologist and provides care specializing in pregnancy, labor, birth, and the reproductive system.
Obstetrician
A medical doctor who provides care specializing in pregnancy, labor, and birth.
Open enrollment period
The specific days each year during which you can make changes to your
health plan coverage for the next plan year.
Opioids
A class of drugs that help to reduce pain is prescribed by a medical provider. Learn more about opioids and pregnancy.
Outpatient
A patient who receives health care services without overnight admission to a
hospital or other medical facility. Outpatient care may be provided in a
physician’s office, a clinic, the patient’s home, or an
emergency room.
P
Participating provider
A doctor, hospital, pharmacy, lab, or health center that has a
contract with HMSA to charge set rates for services or products.
Seeing these providers is almost always cheaper than using
nonparticipating providers.
Payment determination criteria
Criteria HMSA is required by Hawaii law to use to determine if a service or
supply is medically necessary.
Pneumococcal
Related to a bacterium of the genus Streptococcus (S. pneumoniae)
that causes the most common and severe forms of pneumonia, an infection of
one or both lungs.
Postpartum
Refers to the time after giving birth.
Postpartum depression
Also called postnatal depression, a type of depression that affects
10 percent of women who give birth or have a miscarriage.
It may interfere with the mother’s ability to care for her baby and
handle other daily tasks.
Precertification
Approval process used before certain services and supplies are rendered to ensure that the services or supplies are covered services.
Preconception care
The care you receive before getting pregnant. Your doctor makes sure that you’re healthy and your body is ready to get pregnant.
Preeclampsia
A serious health condition that can develop from the 20th week of pregnancy until after giving birth (postpartum preeclampsia). It causes high blood pressure and kidney and liver dysfunction. If gone untreated, it can cause serious health problems for you and your baby. However, most people with preeclampsia have healthy babies if it’s addressed in a timely manner. Some signs and symptoms of preeclampsia are headache that doesn’t go away; pain in your upper right belly area under your ribs (where your liver is located); blurred vision; seeing flashing lights; seeing spots; light sensitivity; severe nausea and/or vomiting; swelling in hands, legs, and/or face; and rapid weight gain (two to five pounds in a week). More on preeclampsia.
Preferred brand drug
A brand drug that has a preferred brand status on an HMSA prescription
drug formulary. You may incur a higher copayment for a preferred drug
than a generic drug.
Preferred provider organization (PPO)
A type of health plan that allows you to choose any health care provider.
Providers within the network agree to accept HMSA’s
eligible charge,
minus your copayment, as payment in full. Nonparticipating providers
haven’t agreed to accept HMSA’s eligible charge as payment in full.
If you receive services from a nonparticipating provider,
you owe a copayment plus the difference between the nonparticipating
provider’s billed charge and HMSA’s eligible charge.
Premature baby (or preterm baby)
A baby born too early, before 37 weeks of pregnancy.
Premium
A monthly payment you make to your health insurer for your health plan.
Your employer may pay part or all of the premium.
Prenatal
Refers to the time before giving birth, the time during pregnancy.
Prepaid credit card
You can use this stored-value card to make purchases or get cash you have
deposited into the card’s account. Since the card is endorsed by a
credit card company, you can use it anywhere credit cards may be used.
Also, there’s no interest charges because you aren’t borrowing
money from a financial institution.
Pre-pregnancy
The stage also known as preconception; the period before and between pregnancies.
Preventive care
Services for early detection and treatment of diseases.
It also includes programs that promote healthful lifestyles through
immunizations, workshops, counseling, and education.
Primary care
General medical care that focuses on
preventive care
and the treatment of routine injuries and illnesses.
Primary care provider (PCP)
A physician or other health care provider who treats you for common illnesses,
manages your preventive care and well-being, and refers you to a specialist
when necessary. It's ideal to establish a long-term relationship with a
PCP to get the best care.
Q
Qualifying event
An occurrence (for example: death, termination of employment, or change in
family status, such as divorce) that changes a former employee’s
eligibility status under a group health plan. The term is used in
reference to COBRA eligibility.
R
Referral
In some health plans, such as an
HMO,
if the PCP
determines that a patient’s condition requires the services
of a specialist or facility, the PCP arranges for the patient to
receive the necessary care from the appropriate provider to ensure
the services are covered.
Refractive eye surgery
Corrective laser eye surgery.
This includes reshaping the cornea with a laser (PRK or LASEK) or
reshaping the cornea with an incision and a laser (LASIK®).
Report to Member
A narrative or claim determination (payment or denial) that’s sent
to the subscriber or specific dependent of an HMSA account when a claim
is processed. The Report to Member may also be known as an Explanation
of Benefits.
S
Screening
Testing for early detection of a specific disease in individuals without
signs or symptoms of the disease.
Secure message
A private way for you to send and receive messages that prevents messages
from being intercepted by someone other than the intended recipient.
Secure messages help protect information such as
confidential member information.
Security code
A feature for credit or debit card transactions that gives increased protection
from fraud. On MasterCard, Visa, and Discover credit or debit cards,
it typically consists of three digits printed on the back of the card,
to the right of the signature strip. On American Express cards, it is
four digits printed on the front of the card, on the right side.
Sexually transmitted infections (STIs)
Also commonly known as sexually transmitted diseases (STDs), they’re infections that are passed from one person to another through sexual contact. These infections are generally contracted through vaginal, oral, or anal sex, but could also be spread through contact with the penis, vagina, mouth, or anus. There are more than 20 types of STIs. The most common types are chlamydia, gonorrhea, HIV, herpes, syphilis, bacterial vaginosis, and trichomoniasis. STIs could be passed to your baby during pregnancy or when you give birth. STIs could also be passed by breastfeeding, blood transfusions, or sharing needles. More information about STIs.
Single plan
A health plan that covers just one person with no dependents.
Single-source generic drug
A single-source generic drug is a generic drug that is more expensive
than other generics because only one manufacturer makes it.
Skilled nursing facility (SNF)
A licensed facility that provides
inpatient nursing care and
rehabilitation services for patients who don’t require
hospitalization for an acute condition. At an SNF, an on-call physician and
registered nurse are available 24 hours a day.
Specialist
A provider who is specifically trained in a certain branch of medicine
related to a service or procedure, body area or function, or disease.
Spina bifida
A type of neural tube defect and can happen anywhere along the spine if the neural tube doesn’t close all the way during fetal development. The backbone that usually protects the spinal cord and nerves doesn’t properly form. The spinal cord and nerves can become damaged and may cause physical and intellectual disabilities that range from mild to severe. Learn about the common types of spina bifida.
Stillbirth
When a baby dies in utero after 20 weeks of gestation. Still births could also happen during labor. Still births can happen to anyone and there are risk factors that can make chances of still births occur. For example, smoking, drug abuse (recreational and prescription), being obese, having high blood pressure, and diabetes can heighten chances of having a still birth. Learn more about still births.
Subscriber
The person who fills out the enrollment form and is covered by an individual
plan or an employer’s group insurance policy or health plan. If the
plan allows family coverage, the
subscriber (policy holder) may also enroll eligible
dependents in the plan.
Sudden unexpected infant death syndrome (SUID) and sudden infant death syndrome (SIDS)
SUID is the sudden unexpected death of a baby before their first birthday when the cause of death wasn’t obvious before investigation. SUID include SIDS, accidental suffocation while sleeping in whichever sleeping environment, and other unknown causes of death. Learn more about SUID and SIDS.
Supplemental insurance
Extra insurance for medical expenses that aren’t a benefit of your health plan.
This could include chiropractic care and acupuncture.
Supplements
Are vitamins, minerals, herbs, and many other food-type products. Supplements aren’t used to replace food, but to add to your daily diet. Some supplements could be beneficial for your health and should always be reviewed by your health care provider before taking.
U
Urgent care
Medical care for an unexpected illness or injury that isn’t
life-threatening but can’t wait until the patient visits a
PCP.
V
Vaccination
Getting a vaccine or vaccines to obtain protection form specific diseases. This term is used interchangeably with immunization.
Vitamins
Found in the food that we eat daily, which helps the cells in our body to properly function and keep us healthy. It’s important to have an adequate amount of vitamins in our body.
W
Well-woman exam
A gynecological examination that typically includes a pelvic exam,
a collection of a specimen for Pap smear screening, and a clinical breast exam.